The field of cell engager therapeutics, particularly T cell engagers (TCEs), has witnessed remarkable growth in recent years. With a surge in approvals and expanding clinical applications, these agents are reshaping the landscape of cancer immunotherapy. Yet, as the science advances, so too do the complexities and challenges associated with their clinical deployment. This article explores the multifaceted clinical challenges in the application of cell engagers, drawing on recent expert panel discussions, and looks ahead to the innovations and strategies poised to address these hurdles.
The Promise and Progress of T Cell Engagers
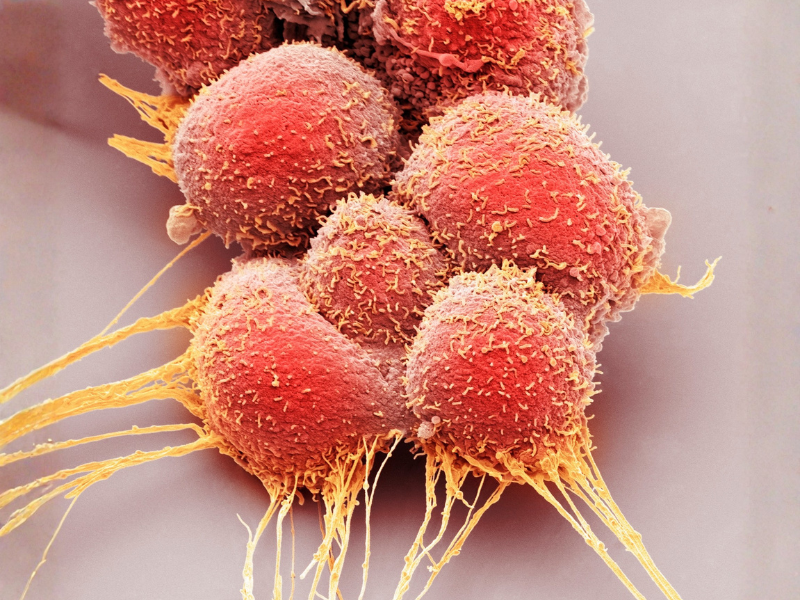
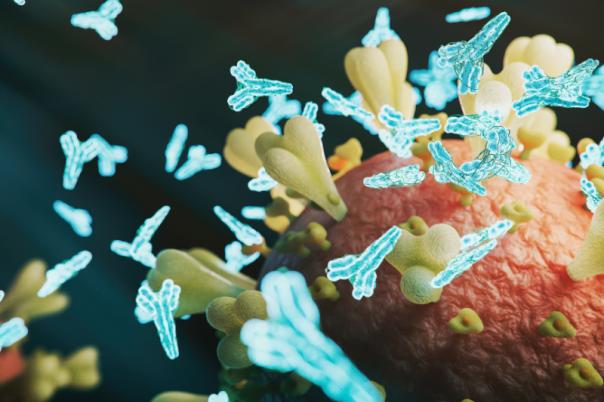
T cell engagers are engineered molecules designed to redirect T cells to recognise and eliminate cancer cells. Their mechanism – bridging T cells and tumour cells via dual antigen recognition – has led to significant successes, particularly in hematologic malignancies. As of 2025, eleven TCEs have received regulatory approval, with the majority targeting haematological cancers. Notably, several agents focus on the same antigens, such as BCMA and CD20, reflecting both the promise and the limitations of current target selection strategies.
While these successes are encouraging, the translation of TCEs to solid tumours remains a formidable challenge. The heterogeneity of antigen expression, tumour microenvironment barriers, and the need for precise target selection complicate the development of effective and safe TCEs for solid tumours. The field is thus at a pivotal juncture, balancing optimism with the realities of clinical translation.
Key Clinical Challenges
1. Target Selection and Antigen Heterogeneity
One of the foremost challenges in TCE development is identifying suitable tumour antigens. In hematologic cancers, certain antigens are relatively tumour-selective, enabling more straightforward targeting. However, in solid tumours, antigen expression is often heterogeneous, and many potential targets are also present on normal tissues, raising the risk of off-tumour toxicity.
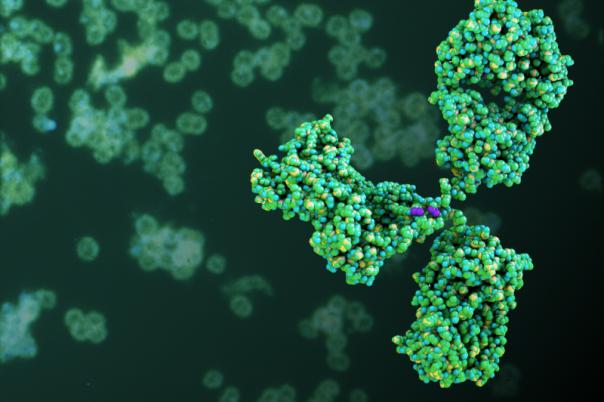
The selection of “clean” targets – those with high tumour specificity and minimal normal tissue expression – is critical but rare. Engineering approaches, such as the development of bispecific or multi-specific engagers, aim to improve selectivity, but these innovations introduce additional layers of complexity in design, manufacturing, and clinical evaluation.
2. Potency and Efficacy: The CD3 Affinity Dilemma
Determining the optimal potency of the CD3-binding arm of TCEs is another nuanced challenge. While lower-affinity CD3 binders may reduce the risk of cytokine release syndrome (CRS) and other toxicities, they may also compromise efficacy, particularly in solid tumours where T cell infiltration and activation are already suboptimal. Conversely, high-affinity binders may enhance efficacy but at the cost of increased toxicity.
The field is moving toward a more sophisticated understanding of the “Goldilocks zone” for CD3 affinity – potent enough to drive anti-tumour responses, but not so strong as to provoke unacceptable adverse events. This balance is further complicated by differences in tumour burden, microenvironment, and patient-specific factors.
3. Preclinical Modelling and Predictive Limitations
Translating preclinical findings into clinical success remains a persistent hurdle. Traditional in vitro and in vivo models often fail to fully recapitulate the complexity of human tumours and immune responses. For example, while xenograft and patient-derived xenograft (PDX) models provide valuable insights, they may not accurately predict efficacy or toxicity in patients.
Companies are increasingly employing a combination of models – xenograft, syngeneic, and in vitro assays – to capture a broader spectrum of tumour biology and immune interactions. However, no single model is sufficient, and the predictive value of these systems for clinical outcomes, particularly for CRS and immunogenicity, remains limited. Reverse translational studies, where clinical data inform model refinement, are becoming more common, but the gap between preclinical promise and clinical reality persists.
4. Pharmacokinetics, Immunogenicity, and Manufacturing
TCEs present unique pharmacokinetic (PK) challenges, including target-mediated drug disposition (TMDD) and variable half-lives. Predicting human PK from animal models is fraught with uncertainty, and multiple approaches – such as using transgenic models and parallel PK studies – are often required to mitigate risks.
Immunogenicity, particularly the development of anti-drug antibodies (ADAs), is a significant concern. TCEs, by their mechanism, activate T cells and can provoke higher ADA incidence compared to other biologics. While in silico and in vitro assays can help predict immunogenicity risk during candidate selection, these tools are imperfect, and clinical mitigation strategies – such as pre-treatment with B cell depleters – may be necessary. Manufacturing complexities, including the need to monitor for product-related impurities and ensure batch consistency, add further layers of challenge.
5. Safety: Cytokine Release Syndrome and Neurotoxicity
CRS and neurotoxicity are among the most serious adverse events associated with TCEs. Predicting and managing these toxicities is a major focus of both preclinical and clinical development. While lower-affinity CD3 binders and step-up dosing regimens can reduce risk, they may also impact efficacy. The development of predictive biomarkers and improved preclinical models for CRS is an active area of research, but definitive solutions remain elusive.
Innovations and Future Directions
Despite these challenges, the field is advancing rapidly, with several promising strategies on the horizon:
1. Next-Generation Engineering
Novel formats, such as multi-specific engagers (e.g., “two-plus-one” designs) and conditional activation systems, are being developed to enhance selectivity and reduce off-tumour effects. Costimulatory approaches, where TCEs are combined with agents that provide additional T cell activation signals, are also under investigation. These innovations aim to overcome the limitations of current TCEs and expand their applicability to more tumour types.
2. Integrated Risk-Benefit Assessment
Regulatory agencies are increasingly requiring integrated summaries of immunogenicity and risk mitigation strategies, even at early stages of development. This shift is driving a more holistic approach to candidate selection, where efficacy, safety, manufacturability, and immunogenicity are weighed together. The use of real-world data and adaptive trial designs may further enhance the ability to identify and manage risks in clinical development.
3. Personalised and Adaptive Approaches
As understanding of tumour biology and immune responses deepens, there is growing interest in personalising TCE therapy. Biomarker-driven patient selection, adaptive dosing strategies, and combination regimens tailored to individual risk profiles are likely to become more common. These approaches hold promise for maximising benefit while minimising harm.
4. Collaborative and Cross-Disciplinary Research
The complexity of TCE development necessitates collaboration across disciplines – immunology, oncology, bioengineering, regulatory science, and manufacturing. Cross-company and academic partnerships, as well as engagement with regulatory agencies, are essential for advancing the field and overcoming shared challenges.
Conclusion
The application of cell engagers, particularly T cell engagers, represents a frontier in cancer immunotherapy. While significant progress has been made, numerous clinical challenges remain, spanning target selection, potency optimisation, preclinical modelling, pharmacokinetics, immunogenicity, and safety. The field is responding with innovation, collaboration, and a commitment to integrated risk-benefit assessment.
Looking forward, the continued evolution of engineering strategies, predictive models, and personalised approaches promises to unlock the full potential of cell engagers. As the science advances, so too will the ability to deliver safe, effective, and durable therapies for patients with cancer and beyond. The journey is ongoing, but the future of cell engager therapeutics is bright, shaped by both the lessons of today and the innovations of tomorrow.