Key Takeaways:
- Gene therapy restored immune function in 59 of 62 children with ADA-SCID.
- ADA-SCID is a severe, often deadly immune disorder in infants.
- Standard treatments have major limitations.
- The therapy uses a lentiviral vector to deliver a working ADA gene.
- Immune function remained stable long-term, with no serious complications.
- Three children needed alternative treatments.
- FDA approval is being pursued; commercial manufacturing is next.
A gene therapy has restored lasting immune system function to 59 out of 62 children with ADA-SCID, a rare genetic immune disorder. The experimental therapy was given as part of a study conducted by the University of California Los Angeles, University College London, and Great Ormond Street Hospital.
ADA-SCID
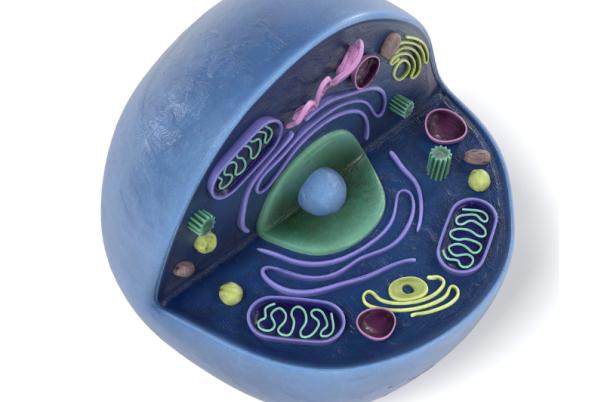
Severe combined immunodeficiency due to adenosine deaminase deficiency (ADA-SCID), is a rare and deadly immune disorder that is caused by mutations in the ADA gene. ADA encodes for the enzyme adenosine deaminase which is essential for the immune system to function.
ADA-SCID accounts for about 10-20% of severe combined immunodeficiencies. Typically presenting in infants in the first 6 months of life, the disorder is deadly if left untreated.
The standard available treatments include bone marrow transplantation or enzyme replacement therapy. Both come with limitations, the former relies on finding a matched donor, preferably a sibling, and the latter requires weekly injections to maintain effectiveness.
Gene therapy: a new approach
The new approach, tested by UCLA, UCL, and Great Ormond Street, took blood stem cells from the participants and used a lentiviral vector to deliver a working copy of the ADA gene. When the fixed cells were reinfused into the patient’s bloodstream, they were able to proliferate and produce healthy immune cells, restoring immune function.
“These results are what we hoped for”
This study is the largest and longest of its kind, tracking 474 patient-years, including five patients treated over ten years ago. Among the 59 successfully treated patients, immune function has stayed stable beyond recovery, with no serious complications reported.
Donald Kohn is a distinguished professor at UCLA, and senior author on the paper which was published in the New England Journal of Medicine.
He said: “What’s most remarkable is that everything has been completely stable beyond the initial three-to-six-month recovery period. Treatment was successful in all but three of the 62 cases, and all of those children were able to return to current standard-of-care therapies.”
Two of those patients received bone marrow transplants, and one patient was undergoing ADA enzyme injections in preparation for a transplant.
“These results are what we hoped for when we first began developing this approach. The durability of immune function, the consistency over time and the continued safety profile are all incredibly encouraging,” said Kohn.
Next Step: FDA Approval
The team at UCLA are now seeking FDA approval for their gene therapy approach. LA-based biotech company Rarity PBC has now licenced the therapy and is searching for pharma manufacturing collaborators.
“Our goal is to have this therapy FDA-approved within two to three years,” Kohn said. “The clinical data strongly supports approval — now we need to demonstrate that we can manufacture the treatment under commercial pharmaceutical standards.”